4 Practical Ideas for Reducing Patient Interruptions and Why It Matters
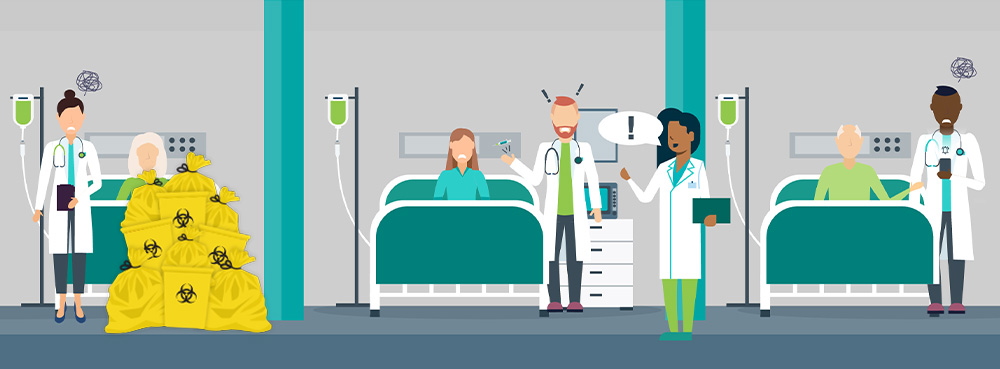
Canadian medical facilities are busy, fast-paced environments where clinicians are hard at work trying to improve patient outcomes. Unfortunately, these environments naturally create a lot of potential for interruptions. Some of these are necessary, but others can simply lead to stress and a high potential for errors.
Patient interruptions occur when a clinician is drawn away from one task, such as prescribing treatment or administering medications to a different task. This creates a distraction that can result in errors and potential threats to patient safety.
Distractions are ubiquitous in our modern lives. So, it’s easy to see them as little more than a nuisance. But when it comes to healthcare, the risks of devastating mistakes are high. So, let’s take a look at why reducing interruptions is so important and some simple steps facilities can immediately take to reduce and, in some cases, eliminate the sources of these distractions.
TOPICS WE WILL COVER:
1 / Why Is It Important To Reduce Patient Interruptions?
2 / What Can Healthcare Providers Do To Eliminate Patient Interruptions?
Why Is It Important To Reduce Patient Interruptions?
Interruptions and multitasking have simply been accepted as a normal part of working in a healthcare environment in many facilities. However, these interruptions can have severe consequences, not only for practitioners who face increasing stress and mental fatigue juggling several tasks at once, but for patients as well. 
After returning from an interruption, practitioners may fail to remember where they left off on a task. One of the most significant and best-studied impacts of these distractions comes from interruptions during the preparation and administration of medications.
The Canadian Adverse Events study found that drug- and fluid-related events were the second most common type of adverse healthcare events. Providing more context on the cost of these errors, the Institute of Medicine found that 450,000 medication errors occur every year. These are estimated to have an annual cost of $3.5 to $29 billion annually. Even more troubling is that these events can cause thousands of unnecessary deaths, a truly sobering statistic.
In fact, this is so common that studies have shown that medical professionals such as pharmacists, technicians, and nurses are interrupted as frequently as once every two minutes while dispensing and administering medications. Another study found that nurses were interrupted at least 65.5% of the time when completing these medication tasks.
In some cases, interruptions are essential for patient safety. For example, sometimes a patient will question a nurse because they are unaware of why they are receiving medication. However, in many cases, interruptions are avoidable, such as those caused by other healthcare staff inquiring about information that could be gained from a patient’s medical records.
Poorly timed interruptions can cause critical harm. Studies show that each time a nurse is interrupted, the risks of error can increase by up to 12%. Other reports have found that an increased frequency of errors can correspondingly result in increased severity of errors.
What Can Healthcare Providers Do To Eliminate Patient Interruptions?
What the information above clearly shows is the importance of reducing or eliminating patient interruptions. But this is often a difficult challenge. Interruptions come in many forms, including staff movement in and out of rooms, loud noises, and direct interactions with providers. However, there are some steps that healthcare providers can immediately take to prevent interruptions without lengthy research or training. We will take a close look at each of these strategies below.
No Interruption Zones

The “No Interruption Zone” strategy is a strategy borrowed from aviation’s sterile cockpit rule. This rule bars non-essential activities during critical phases of flight. Just like its inspiration, when a nurse or other healthcare provider is inside the no-interruption zone, other staff know not to distract them.
This zone could be demarcated around patient care areas or any other zones where critical processes take place. A particular implementation of the no-interruption zone that has shown promise is creating such a zone around medication carts. By instructing healthcare staff that nurses are not to be interrupted in an invisible zone around medication carts or charting, the McGill University Health Centre has reduced medication errors by 60%.
This method can eliminate many of the most common and severe interruptions, such as staff approaching for questions. Additionally, in certain cases, it can reduce staff movement in and out of protected spaces. This practice may also benefit if coupled with strategies to remove mobile devices, such as pagers, cell phones, and other sources of interruptions.
Do Not Disturb Vests
Do not disturb vests or an equivalent symbol can function very similarly to the “Do Not Disturb” zone. However, it can have additional benefits for those who are unfamiliar with any demarcated zones. If the vest is clearly labelled, it can inform surrounding staff that they are not accessible with less risk that individuals may be unaware of the program.
This is a simple solution that can be implemented immediately with little training or preparation. It does have drawbacks, however, as it may have little effect on entrances or exits from working spaces. It may also send the wrong message to patients. Some patients may think they should avoid asking nurses for assistance while they are wearing the vest. Regardless, these vests can send a clear and effective message that can help to reduce staff interruptions during critical tasks.
Protected Hours
Another effective strategy is the “protected hour,” during which designated staff can focus exclusively on their critical tasks. This method has the advantage that staff can plan to avoid any interruptions during this period, which includes reducing noise, movements between critical work areas, and informing callers that the individual is unavailable.
One study found that such a policy could increase the correct dosing of medications by 11% over the baseline. This type of policy can be highly effective, but it is limited to only a specific timeframe. Therefore, it will have no effect on critical activities occurring outside of the designated time frame.
Improved Waste Management
Staff must take time away from their other responsibilities to properly dispose of medical waste. This not only slows them down but also creates a new window for patients to interrupt their workflow. However, if the number of steps and complications in the waste disposal process is decreased, it will minimise patient interruptions and save time. Moreover, an optimised waste disposal strategy reduces injuries, another common source of wasted time and resources. Simple ways to improve a facility’s waste disposal plan include placing containers at the points of waste generation and ensuring they are the right size and clearly colour-coded for the right variety of waste.
Wall-mounted bins for sharps or certain other waste types are a practical choice that can be installed right where the usage occurs. For other needs, mobile containers can be wheeled to wherever staff can most benefit from them. Containers designed for hands-free usage are a boon for quick-moving clinicians. They allow staff to immediately trash certain items without having to go far to utilise the waste receptacle. This minimises time spent on disposal and, therefore, time at risk of patient interruptions.
Colour-coding is a step that guarantees all waste can go towards the correct stream for disposal without staff needing to think twice about it. Sharps, biomedical waste, pharmaceuticals, and more require specialised methods of elimination. But that is a worry for a facility’s waste disposal provider, not onsite staff. Members of the staff should be able to tell the proper bin at a glance.
Partnering with an experienced waste disposal service is the fastest way to spot inefficiencies in a facility’s current strategy and optimise the entire team’s waste disposal duties. Daniels Health has revolutionised the practical aspects of waste disposal for real world applications. Utilising a unique “Four Walls” strategy for recommending improvements to waste strategies, Daniels waste experts evaluate a facility’s existing processes, all the way down to each step staff members take to reach a bin, as well as auditing all waste streams created and how bins are currently used.
Based on these data, Daniels creates a comprehensive strategy for improving a facility’s waste strategy. Daniels’ team provides training to staff on proper usage of any new containers, compliance, and more. This one step can save significant time and have a dramatic effect to reduce patient interruptions. Choosing Daniels as a waste disposal partner guarantees that the burden of waste management is minimised for staff.
